Whenever you see lots of advertising, or hear something frequently, it means there is ample money in it. Thus, screening for cancer is important. All stress how essential it is to search for cancers. The idea is to find a cancer when it is small, and then be able to remove it entirely before it spreads all over the body. Screening for colon cancer is especially promoted. People are being pushed and even bullied into getting a colonoscopy. The risks and benefits are not discussed, or if it is an option, but rather forced into the procedure.
So, I would like to present you with what a doctor should give you to make a wise decision for yourself.
What is a Colonoscopy?
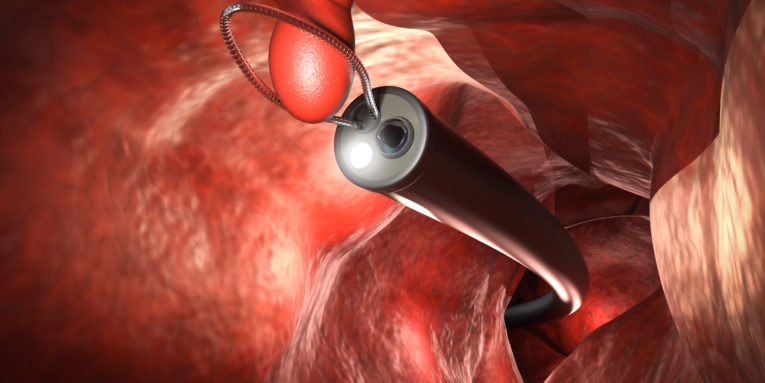
A colonoscopy is putting a long fiberoptic camera through the anus into the rectum for the doctor to visually see the colon. It requires a cleanse called a “bowel prep” to make sure the colon is “squeaky-clean.” This allows the doctor to see the lining of the colon, and any polyps that might be there. If there are any “suspicious lesions,” the doctor can remove them or do a biopsy and send them to the pathologist to determine if there is cancer.
When doctors recommend colonoscopy, they generally quote the benefits without acknowledging the risks, so we will address the risks.
COLONOSCOPY RISKS
Colonoscopy does not see all lesions because not all are apparent. A good colonoscopist will miss about 30% of the lesions. Some miss over 60%! Colonoscopy is thus an incomplete test.[1] This leads to about 9% of those screened by a colonoscopy developing colorectal cancer in the ten years before their next test.[2] That’s about equivalent to the general population.
There is only one prospective randomized trial comparing colonoscopy to doing nothing. Last year, The New England Journal of Medicine published a European trial of colonoscopy that showed an 18% decreased risk of dying from colon cancer in the population offered screening, but the overall death rate stayed the same.[3] There is no evidence that colon cancer screening will lower the overall mortality, so you should not be told, “It could save your life.”
What’s worse is that the procedure itself has risks. Serious complications include bleeding and perforation with infection in the abdomen, which seems to be around 28 per ten thousand colonoscopies performed.[4] The chances of harm from the procedure are not small. Serious bleeding can occur from removing a polyp, about 50 per ten thousand, depending on the study. And death from perforation is around 5 per ten thousand.[5] If you consider the low rate of colon cancer, these complications are significant.
It is important that you understand the numbers. Colon cancer is not a big cause of death. The overall odds of dying from colon cancer are one in ten thousand in the United States[6] It requires over a thousand screening colonoscopies to find one cancer. Moreover, three colon cancers are diagnosed for everyone who dies from the disease, so most are not deadly. The low rate (3.6 per ten thousand) of this cancer makes screening difficult. Therefore, the death rate from colonoscopy is significantly higher than the death rate from colon cancer. Screening for colon cancer has not changed the death rate from colon cancer over the population. In fact, it’s increasing.
Other complications are not from the test, but from the bowel cleanse or anesthesia administered for the test. I have had several patients with bowel prep issues, including chronic diarrhea afterwards.
Thus, it may be riskier to do the test than to get the cancer. The bottom-line is there is risk to the procedure that is greater than the potential or tested benefits. If you are going to get a colonoscopy, you may need to determine if this is valuable. For example, if you have bleeding, colitis, hereditary polyposis, Lynch syndrome, obstruction, or some other colon abnormality, you may need a colonoscopy. Doing a diagnostic colonoscopy is useful because though the risks are still there, they are clearly worth the benefits. However, screening healthy people is riskier because there is so little benefit.
OTHER HELPFUL TESTS
There is no good test that detects most colorectal cancers. Even though colonoscopy misses about 50% of cancers, it is still considered the standard of screening tests for colon cancers. However, there are other types of tests that might be appropriate. They include:
Stool Blood Test (FIT)
This test looks for blood in the stool. If the test is positive, then do a colonoscopy. This is not at all accurate either for finding cancer you already have, nor to determine that you don’t have cancer. If it comes up positive, then you need a colonoscopy. But it is the most cost-effective test available, with a benefit equivalent to the other tests.
FIT-DNA test
The FIT-DNA test looks for altered DNA, which may indicate a cancer. Again, get a colonoscopy if it comes up positive. This test is almost as good as the FIT test because it is done every three years. The FIT is better and less expensive.[7] (This is the “Cologuard” test.)
Sigmoidoscopy
A sigmoidoscopy is a shorter scope that only looks at the last third of your descending colon, or the sigmoid colon. Since most colon cancers are in this part, it has about the same decrease in colon cancer with significantly less risk.[8] I would prefer this over a colonoscopy not just because the risks are significantly lower, but also because the bowel prep is much easier (an enema) and it doesn’t require sedation.
Virtual Colonoscopy
This test uses a CT scan with contrast to generate images of the colon. This test doesn’t see small lesions and is not able to do any biopsies. It misses about 50% of lesions, similar to a colonoscopy, but different ones.
Of all these options, I suspect that I would choose the FIT test for screening, and a sigmoidoscopy if there were anything positive. I would do a colonoscopy only, if necessary, for example, if there are multiple polyps or the cause of bleeding is not found with sigmoidoscopy.
What To Do Instead of Screening
Exercise
The strongest association to colorectal cancer is activity level. More activity means less death from colorectal cancer.[9] An analysis of 126 studies on cancer show decrease of 19% in those who are most physically active compared to the couch-potatoes, which is as good as any cancer screening. However, even this may not consider that those who are more physically active may have better diets and take their vitamins, so it may not be just activity.
Diet
(There is a lot of conflicting information because of the difficulties of doing research on diet. The following is the best I can find.) Eating a high vegetable diet with fish (pescavegetarian) may decrease the risk of colon cancer by as much as 43%.[10]
One study showed that high vegetable with low meat consumption compared to high meat and low vegetable consumption was associated with 8 times lower rate of colon cancer.[11] Interestingly, taking meat away from those who ate it seemed to be more protective than adding vegetables. Another study showed that it wasn’t just any meat, but processed meats like salami and hot dogs, may be related to colon cancer.[12] They further found that the marker for cancer “wasn’t associated with diets high in chicken or fish. It also wasn’t associated with other lifestyle factors such as smoking, high body mass index, or high alcohol consumption.”
So, what is the best diet? Probably the one that works best for you, to prevent constipation or inflammation. Some people don’t tolerate tomatoes, for example, and should avoid them. And, though milk is associated with a lower rate of colon cancer (see xvii) it can cause constipation or diarrhea in some people.
That said, there is one dietary intervention that clearly decreases colorectal cancer risk, and is even an effective treatment for those who already have it.[13] [14] Fasting. Fasting means “empty stomach.” This is not eating small amounts, drinking juice, broth, or even water. It means nothing in the mouth (including chewing gum). Intermittent fasting has a wonderful effect on the prevention of cancer. The benefits accrue the longer a fast is maintained. Intermittent fasting is a great way to prevent cancer of the colon.[15] Some ideas to consider for how long to fast:
- Eat 2 meals per day: 7:00am and 3:00pm gives you a 16 hour fast and keeps a perfect circadian rhythm. If you do this 5 days per week, it gives you some room for social eating.
- Fast 3 days every month, drinking water only when you are thirsty.
- Fast for seven days twice per year with only water when you are thirsty.
Vitamin D
There is good evidence that the level of vitamin D is associated with lower risk of dying from colorectal cancer.[16] One study indicated high vitamin D intake from food offered a 50% lower risk from colorectal cancer in people under 50.[17] Even if the numbers are a little off, I think getting enough vitamin D is helpful.
Selenium
Several studies have shown that high selenium diets are associated with lower risk of colorectal cancer. One interventional study showed a 61% lower risk.[18] These used high-selenium yeast because that is an organic form that is easily absorbed. Do not take too much – about 200mcg per day is adequate – because high selenium can cause cancer as well.
Recommendations
- FIT stool blood test annually
- Exercise regularly
- High fiber diet
- Avoid processed meats
- Fast periodically
- Vitamin D3 10,000 IU per day
- Selenium 200mcg per day
These measures are not only to screen for a cancer you already have, but rather to prevent you from ever getting it. Protecting your colon is by FAR better than finding a cancer early. The numbers are clearly better for exercise, diet, fasting and nutrition than for screening tests. Again, if you are screening for cancer, you are looking for one that is already there. It is so much better to avoid it entirely.
Dr.Scott Saunders M.D.