Controlling When You Have to Go to the Bathroom – NATURALLY
Several years after her surgery, Marge began having frequent urinary tract infections. Eventually, she had a cystoscopy. The surgeon looked into the bladder and found what she had feared – mesh. The plastic mesh placed to suspend Marge’s bladder had worn through the wall of the bladder, creating inflammation and infection. She needed surgery to remove the mesh. The problem, however, was that tissue had grown around the mesh. As expected, scar tissue formed to protect the body from the foreign material. The entire mesh sling was no longer a separate piece of plastic that could be removed. It had become an integral part of the pelvic organs from the skin to the bladder, and even the uterus and ovaries.
After three surgeries she was better – for a while. But more mesh was found that had been missed. She continues to have chronic bladder problems.
It all started when Marge was having urinary incontinence and went to the doctor. They looked at the options. Medications weren’t very helpful, though they did improve the urgency to go. Finally, they settled on a surgical procedure called a sling that would pull the bladder up, so the tube (urethra) wasn’t “kinked.” This procedure has been used for years with good success, and Marge wouldn’t have to take medications. The sling seemed to be the simplest solution, but she didn’t know the potential complications.
Normal urinary function
The urinary system is a beautiful work of complex fluid mechanics and engineering. The kidney pushes urine into the bladder. Under pressure, the bladder stretches to fill like a balloon. Valves prevent urine from going back up into the kidneys. The bladder also has a sphincter to hold in the urine as it fills, preventing it from leaking urine. Normally, the bladder can hold up to 500 milliliters of fluid (about a pint).
The wall of the bladder itself is a muscle that actively contracts to push out the urine when we go to the bathroom. Sometimes it takes a few seconds to develop pressure to make the urine flow. This coordinates with the sphincter at the base holding in the urine, which needs to relax. Most of the time, the muscle in the bladder muscle wall is relaxed, allowing the bladder to fill, and the sphincter is tight, preventing leakage. These roles reverse for just a few seconds to let the urine out when we go to the bathroom.
4 Types of Urinary Incontinence
The word incontinence means the inability to hold urine. Sometimes the system doesn’t function properly and urine leaks at unexpected times.
Urinary incontinence is the forgotten stepchild of medicine. Nobody wants to talk about it. Most people who have it don’t bring it to the attention of their doctors. They just assume that they are “getting old” and wear pads, pull-ups, or diapers. Most don’t know that there are four distinct types of urinary incontinence.
- Stress incontinence
- Urge incontinence
- Overflow incontinence
- Functional incontinence
I am going to explain each type of incontinence, how you can know which type you have, and what you can do about it. I hope to spare anyone from having unnecessary surgery, and possible complications.
Stress incontinence
Women have stress incontinence much more than men. Urine can leak out when a person laughs, coughs, sneezes, lifts something heavy, or strains in any way. When abdominal pressure pushes against the bladder, a weak urethral sphincter will leak urine.[1]
Its prevalence in women is probably due to pregnancy, which stretches, or tears, the muscles of the pelvis. The weakened muscles don’t produce enough pressure to hold the urine in the bladder as it fills. Moreover, the pelvic muscles that normally hold up the bladder in the pelvis become weak and allow the bladder to “fall.” Adding pressure from the abdomen during any kind of straining pushes the urine through the loosened sphincter.
The treatments for stress incontinence include surgery, such as a sling or bladder neck suspension, or devices to hold the urine in.
Women may be given a “pessary,” a device inserted into the vagina to hold up the bladder. Poise makes one called “Impressa.” Some use a “urethral plug” to stop the urine during exercise, for example.
There are several types of clamps for men that put pressure on the penis, closing the urethra to prevent leaking urine. There is also an “implantable artificial sphincter” for men who have incontinence from having the prostate removed. These should be used after consultation with a urologist.
Ultimately, tightening the pelvic muscles is the key to prevent and treat stress incontinence. Treatments to help strengthen muscle function include:
- Exercise
- Electrical stimulation
- Estrogen
Electrical stimulation is done with surgical insertion of electrodes. Or, there is a vaginally-inserted stimulator called Apex M that can help build the muscles. This could be helpful for women who are unable to do exercises regularly or properly.
Estrogen, in the form of vaginal creams or suppositories, helps improve the tone of the pelvic organs. This requires a prescription. I prefer to use ESTRIOL (E3), a natural weak estrogen that works locally. But some women require ESTRADIOL (E2), a stronger natural estrogen.
Exercising is simple, and can be done anywhere. But these daily exercises require a few months before seeing results. You may have already heard of “Kegel exercises.”
Kegel exercises contract the pelvic muscles to strengthen them and tighten them. Stronger pelvic muscles hold up the bladder and provide support around the sphincter. The exercises are easy, but should be done twice per day for about 3 weeks before seeing any results. The way to learn which muscle to exercise is simply to try to stop the flow of urine while you are urinating. That’s the muscle. The buttocks and pelvis should not move, and the abdomen should stay soft.
Once you learn how, start a schedule of alternating between quick contractions, as fast as you can for ten seconds, and then slow contractions, using more force, for thirty seconds.[2] Keep alternating these for ten minutes in the morning, and ten minutes at night. Or, you can do them anytime as you are sitting, at work, in the car, or in the waiting room in a doctor’s office, for example.
There are other exercises that help stress incontinence. “Core strengthening” exercises such as abdominal, back, and thigh also improve the function of the pelvic muscles. Many people do PILATES or YOGA for good core strength. Simple calisthenics that we all learned in Jr. High school such as sit-ups, push-ups, and leg-lifts are all helpful. I have one patient who watches old Jack Lalanne videos for her private training sessions.
It is essential to have a daily program to see results. Occasional forays into a gym class won’t suffice.
Urge incontinence
“Overactive bladder” happens when the muscle in the wall of the bladder starts contracting before we’re ready and pushes urine out prematurely. This is a, “When I gotta go…I gotta go NOW!” problem. People who have this know where all the bathrooms are on their route, because they can’t hold it in.
Urge incontinence requires some skill to diagnose. Generally, the bladder contracts too much when it’s irritated. This can happen for many reasons:
- Infection
- Inflammation, such as interstitial cystitis
- Allergies, usually to food, medications, or anything excreted in the urine
- Nervous system damage or inflammation
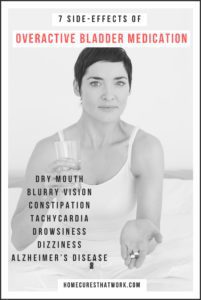
Most doctors will just give medications that relax the bladder to stop the spasms. The problem is that medications don’t just affect the bladder. There are “side-effects” or toxicity from these medications, including:[3]
- Dry mouth
- Blurry vision
- Constipation
- Tachycardia
- Drowsiness
- Dizziness
- And, over time, may contribute to Alzheimer’s Disease
I would avoid these medications, if possible.
Long-term treatment for overactive bladder depends on the cause. Kegel and other exercises can be helpful in holding the urine long enough to get to a bathroom, but may not solve the problem. Often, proper diagnosis requires the help of a doctor to see if you have infections, inflammation, toxins, allergies or nervous system problems. Once the issue is found, the treatment presents itself.
Over the years, I have found the first things to try are diet and exercise. Food sensitivities are a big issue causing inflammation. The “inflammatory mediators” or chemicals created by the food sensitivity reaction are excreted in the urine, sitting in the bladder, causing inflammation, and incontinence.
An “elimination diet” removes foods from your diet to which you might be sensitive for 4 weeks. Then, you add them back slowly to see if you react. The key is within a few weeks of removing the offending foods, the bladder problems should disappear. If they don’t, you need to try other foods, medications, or things ingested. The best way to start the elimination diet is to avoid:
- Gluten
- Dairy
- Nuts
- Seeds
- Nightshades (tomato, potato, peppers, eggplant)
- Sugar
Sometimes just avoiding these will eliminate inflammation and cure many symptoms besides overactive bladder.
Herbs that may help improve bladder function include:
- Angelica archangelica
- Uva ursi
- Pumpkin seed extract
Overflow incontinence
When the sphincter is tightly holding the urine inside the bladder, but the bladder isn’t contracting or there is an obstruction preventing urination, the bladder may continually leak small amounts. The person usually leaks urine unaware. They just find they’re wet, dribbling all the time, but not able to produce a good urine stream or empty the bladder.
The reason this happens is the bladder is overfull because it isn’t draining. Any of the systems could be the cause. Sometimes it is because the bladder wall muscles don’t contract, or the urethral sphincter doesn’t relax. This can happen for several reasons:[iv]
- The nervous system isn’t controlling bladder emptying.
- Diabetes can affect the nervous system.
- Spinal cord injuries can destroy the nerves that control the bladder.
- Multiple Sclerosis, or other disorders of the nervous system.
- Medications either prevent the sphincter from relaxing, or prevent the bladder from contracting.
- Sleeping pills
- Allergy medications
- Narcotic pain relievers
- Incontinence medications
- Blood pressure medications
- Anti-depressants
- There is an obstruction of the bladder outlet, or urethra.
- Men often have prostate enlargement, the most common cause of overflow incontinence.
- Women may have a “fallen bladder” or cystocele that “kinks” the urethra.
- Tumors can cause obstruction of urine flow.
- Sometimes constipation can push against the bladder sphincter, preventing urine flow.
- Scar tissue from damage to the urethra, or surgery can also obstruct the urine.

Treating overflow incontinence requires that you first know the reason why. Each problem has a very different treatment. Some are as simple as stopping or changing a medication, while others require major surgery. Repairing nerve damage may be the most difficult to reverse. But there are ways now, including nutrients, physical therapy, and implanted nerve stimulation. Proper diagnosis usually requires the help of a urologist, a doctor who specializes in the urinary tract.
Men with prostate problems may take medications to relax the prostate and sphincter, allowing better urine flow. Sometimes surgery helps, but it’s just as likely to cause stress incontinence. The best way to avoid this is to exercise, and reduce inflammation.
All of the core-strengthening exercises will be helpful in this. It is essential to remove belly fat for two reasons.
- First, it changes your estrogen-testosterone ratio, which may increase the size of your prostate.
- Second, it mechanically puts pressure on the bladder, which “kinks” the urethra against the enlarged prostate.
For women, sometimes, severe cases of cystocele, rectocele, and uterine prolapse just require surgery to correct. Minor cases may be helped by a pessary. Pelvic floor exercises can still be very helpful, and may eliminate surgery in more mild cases.
Functional incontinence
When people hold their urine for too long, not getting to the bathroom in time, they can lose all, or some, of the urine. This is more common in those who are debilitated in some way and don’t make it to the bathroom in time. Children may have this kind of incontinence when they try to hold the urine too long.
When I was five, my mother put me on a plane by myself to fly from Los Angeles to San Francisco to visit my grandma. I felt the need to urinate soon after the plane took off. But I couldn’t even imagine a toilet on an airplane, so I held it… and held it… until I could hold it no longer. I wet myself, the seat, and everything around! It was VERY embarrassing! (Which is why I remember it so vividly.) That is functional incontinence.
People with dementia may “forget” to go to the bathroom until it’s too late. These people are best put on a schedule to urinate every few hours. The caretaker doesn’t ask if they need to go, they just go on a schedule to avoid “accidents.”
Other Incontinence Treatments and Options
Physical Therapy – A physical therapist who knows how to do pelvic floor therapy can be very helpful for most types of incontinence. I refer everyone with this problem to a physical therapist, even if they are having surgery.
Biofeedback – Training with the various forms of biofeedback can be very helpful for the different types of incontinence. This is a process of becoming aware of your body, and how it functions, helping you to make it function properly.
Homeopathic Formulas – There are several homeopathic formulas for bladder problems. I’m not well-versed in them, but I do have patients who have used them successfully. I look at it like this: It can’t hurt, and it might help!
Heat – There are several new treatments that use heat to “injure” the pelvic tissues, causing a repair response that improves the pelvic area.
- Radiofrequency
- Laser
I have read about these heating therapies, and they seem to work well. But I don’t know if I could recommend them because, while the short-term studies and results are good, I don’t know of any long-term studies. I’m a little wary of damaging tissues to “fix” them.
If you have urine leaking you aren’t just getting old. It is most assuredly NOT inevitable. You do NOT need to suffer with this problem. There are good, safe, and effective ways to prevent and treat almost all the causes of urinary incontinence. It can be complex, and may require the assistance of a good specialist who will look for the cause, but don’t settle for toxic pills. You can improve and even cure your condition so you can have a full and active life. It’s worth the effort to stay continent all your life.
To this end, I have some simple recommendations for any who wish to avoid this problem:
- Exercise regularly, especially core-strengthening, consider Kegel exercises periodically, as well.
- Eat good food, avoid inflammatory foods (sugar, starch, bad fats)
- Don’t allow yourself to get too much fat in the abdomen. If you do, change your diet to remove it. (The Barton Publishing Diabetes Program works well for this).
Beating incontinence isn’t just about what you cut out—try adding in some of these digestive hero ingredients. You might also want to try these exercises to prevent kidney disease or figure out why you need to poop better.
Sources:
1http://www.hopkinsmedicine.org/healthlibrary/conditions/kidney_and_urinary_system_disorders/urinary_incontinence_85,P01528/
2 Kegel AH. Stress incontinence of urine in women: physiologic treatment. J Int Coll Surg 1956;25:487.
3 http://www.health.am/gyneco/urge-urinary-incontinence/
4 http://www.health.am/gyneco/overflow-incontinence/
Article from HomeCuresThatWork.com



