Hypoglycemia, or low blood sugar, is a term that often takes a backseat to the concerns of high blood sugar in individuals with diabetes. However, it is important to shed light on this condition and recognize its significance. So, let’s explore what hypoglycemia really means and why it’s worth knowing about.
The word “hypoglycemia” originates from two components: “hypo” meaning low, and “glycemia” referring to sugar. Essentially, hypoglycemia indicates a state of low blood sugar. But is it really as worrisome as it’s often made out to be? Well, let me share some insights that might change your perspective.
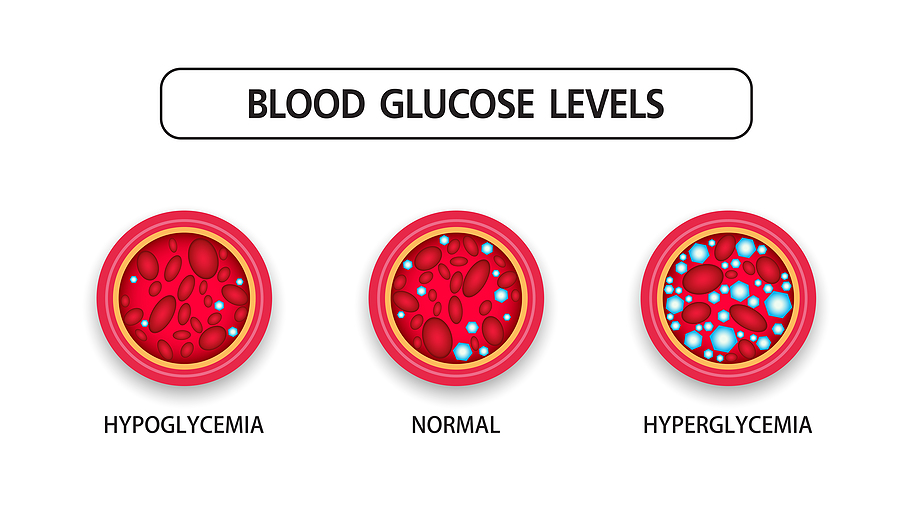
In the realm of diabetes management, the focus is predominantly on high blood sugar levels. We frequently discuss how to keep blood sugar within a target range, and terms like “hyperglycemia” and “elevated A1C” become part of our regular conversations. However, the concept of low blood sugar often takes a backseat.
Contrary to popular belief, mild to moderate hypoglycemia, particularly when blood sugar levels hover around the 50s and 40s, may not be as problematic as it is assumed to be. People often report symptoms like fatigue, weakness, headaches, and a general feeling of unwellness at these blood sugar levels. However, it’s essential to remember that relative to the high blood sugar levels they are accustomed to, these lower readings may cause temporary discomfort.
To understand why this happens, we need to delve into the biology behind it. Our bodies are incredibly adaptive, and our brains play a vital role in this process. The brain has a protective barrier called the blood-brain barrier that only allows glucose (sugar) to pass through when glucose transport proteins are present. Under conditions of consistently high blood sugar, the brain requires fewer transport proteins since there is an abundance of sugar available. However, when blood sugar drops suddenly, the brain may experience a shortage of sugar due to the limited number of transport proteins available.
It is this shortage of sugar reaching the brain that leads to the unpleasant symptoms experienced during hypoglycemia. The brain, being highly dependent on glucose for its energy needs, struggles when blood sugar drops to a level that is relatively lower than what it has become accustomed to. It is important to note that the brain is the primary culprit responsible for the discomfort associated with hypoglycemia.
Now, you might be wondering how to handle hypoglycemia if it occurs. Here’s some advice: it’s best not to follow the conventional approach of consuming orange juice or sugary snacks to rapidly raise your blood sugar. Let’s think about it logically. If you abruptly increase your blood sugar levels, the blood-brain barrier will perceive this surge in sugar availability and respond by producing more glucose transport proteins to transport sugar into the brain. This is precisely what we want to avoid.
Studies conducted on diabetic rats demonstrate this phenomenon. When these rats were intentionally brought into a state of hypoglycemia (around 40), they were kept in this state for several days. By the fourth day, their behavior had returned to normal, even though their blood sugar levels remained low. Further investigation revealed that the blood-brain barrier had produced ten times the usual amount of glucose transport proteins, ultimately allowing for a more efficient sugar uptake by the brain. It takes time for these proteins to be produced and activated, but it is a natural and beneficial process.
Considering all this, hypoglycemia can be seen as a helpful mechanism for increasing the number of glucose transport proteins in our bodies.



